Researching MRSA
Staphylococcus aureus is capable of causing numerous types of infections in humans that range from mild to serious. Indeed, S. aureus can cause minor skin infections such as boils or it can cause more serious infections that result in clinical manifestations such as endocarditis, osteomyelitis, arthritis, septicemia, and toxic shock syndrome, among others, as well as infections of surgical wounds. What is more, S. aureus is known as one of the so-called superbugs, because of the pathogenic nature of the bacterium combined with the fact that it frequently acquires resistance to many currently used antibiotics. Methicillin resistant S. aureus, or MRSA, is one of the most notorious pathogens in the hospital environment and the spread of community acquired MRSA is now becoming prevalent.
The Heinrichs lab investigates the molecular basis of MRSA infections, with a special focus on the mechanisms MRSA uses to acquire growth promoting nutrients, and how these processes govern pathogenicity. Using a wide range of molecular and biochemical tools, the lab aims to answer the following questions:
how does MRSA regulate nutrient source preference?
how does mrsa liberate nutrients from the host?
How does inhibiting nutrient acquisition pathways affect the outcome of MRSA infection?
What are mechanisms by which competing microbes naturally interfere with MRSA?


Select Publications
Goncheva MI, Gibson RM, Shouldice AC, Dikeakos JD, Heinrichs DE. The Staphylococcus aureus protein IsdA increases SARS CoV-2 replication by modulating JAK-STAT signaling. iScience. 2023 Feb 17;26(2):105975. doi: 10.1016/j.isci.2023.105975. Epub 2023 Jan 13. PubMed PMID: 36687318; PubMed Central PMCID: PMC9838083.
Fauerharmel-Nunes T, Flannagan RS, Goncheva MI, Bayer AS, Fowler VG Jr, Chan LC, Yeaman MR, Xiong YQ, Heinrichs DE. MRSA Isolates from Patients with Persistent Bacteremia Generate Nonstable Small Colony Variants In Vitro within Macrophages and Endothelial Cells during Prolonged Vancomycin Exposure. Infect Immun. 2023 Jan 24;91(1):e0042322. doi: 10.1128/iai.00423-22. Epub 2023 Jan 5. PubMed PMID: 36602380; PubMed Central PMCID: PMC9872686.
Chin D, Flannagan RS, Tuffs SW, Chan JK, McCormick JK, Heinrichs DE. Staphylococcus lugdunensis Uses the Agr Regulatory System to Resist Killing by Host Innate Immune Effectors. Infect Immun. 2022 Oct 20;90(10):e0009922. doi: 10.1128/iai.00099-22. Epub 2022 Sep 7. PubMed PMID: 36069592; PubMed Central PMCID: PMC9584346.
Goncheva MI, Chin D, Heinrichs DE. Nucleotide biosynthesis: the base of bacterial pathogenesis. Trends Microbiol. 2022 Aug;30(8):793-804. doi: 10.1016/j.tim.2021.12.007. Epub 2022 Jan 22. Review. PubMed PMID: 35074276.
Flannagan RS, Brozyna JR, Kumar B, Adolf LA, Power JJ, Heilbronner S, Heinrichs DE. In vivo growth of Staphylococcus lugdunensis is facilitated by the concerted function of heme and non-heme iron acquisition mechanisms. J Biol Chem. 2022 May;298(5):101823. doi: 10.1016/j.jbc.2022.101823. Epub 2022 Mar 10. PubMed PMID: 35283192; PubMed Central PMCID: PMC9052147.
Tuffs SW, Goncheva MI, Xu SX, Craig HC, Kasper KJ, Choi J, Flannagan RS, Kerfoot SM, Heinrichs DE, McCormick JK. Superantigens promote Staphylococcus aureus bloodstream infection by eliciting pathogenic interferon-gamma production. Proc Natl Acad Sci U S A. 2022 Feb 22;119(8). doi: 10.1073/pnas.2115987119. PubMed PMID: 35165181; PubMed Central PMCID: PMC8872782.
Batko IZ, Flannagan RS, Guariglia-Oropeza V, Sheldon JR, Heinrichs DE. Heme-Dependent Siderophore Utilization Promotes Iron-Restricted Growth of the Staphylococcus aureus hemB Small-Colony Variant. J Bacteriol. 2021 Nov 19;203(24):e0045821. doi: 10.1128/JB.00458-21. Epub 2021 Oct 4. PubMed PMID: 34606375; PubMed Central PMCID: PMC8604074.
Chin D, Goncheva MI, Flannagan RS, Heinrichs DE. Mutations in a Membrane Permease or hpt Lead to 6-Thioguanine Resistance in Staphylococcus aureus. Antimicrob Agents Chemother. 2021 Aug 17;65(9):e0076021. doi: 10.1128/AAC.00760-21. Epub 2021 Aug 17. PubMed PMID: 34125595; PubMed Central PMCID: PMC8370250.
Chin D, Deecker SR, Ensminger AW, Heinrichs DE. Draft Genome Sequence of Staphylococcus chromogenes ATCC 43764, a Coagulase-Negative Staphylococcus Strain with Antibacterial Potential. Microbiol Resour Announc. 2021 Jun 3;10(22):e0049221. doi: 10.1128/MRA.00492-21. Epub 2021 Jun 3. PubMed PMID: 34080903; PubMed Central PMCID: PMC8354553.
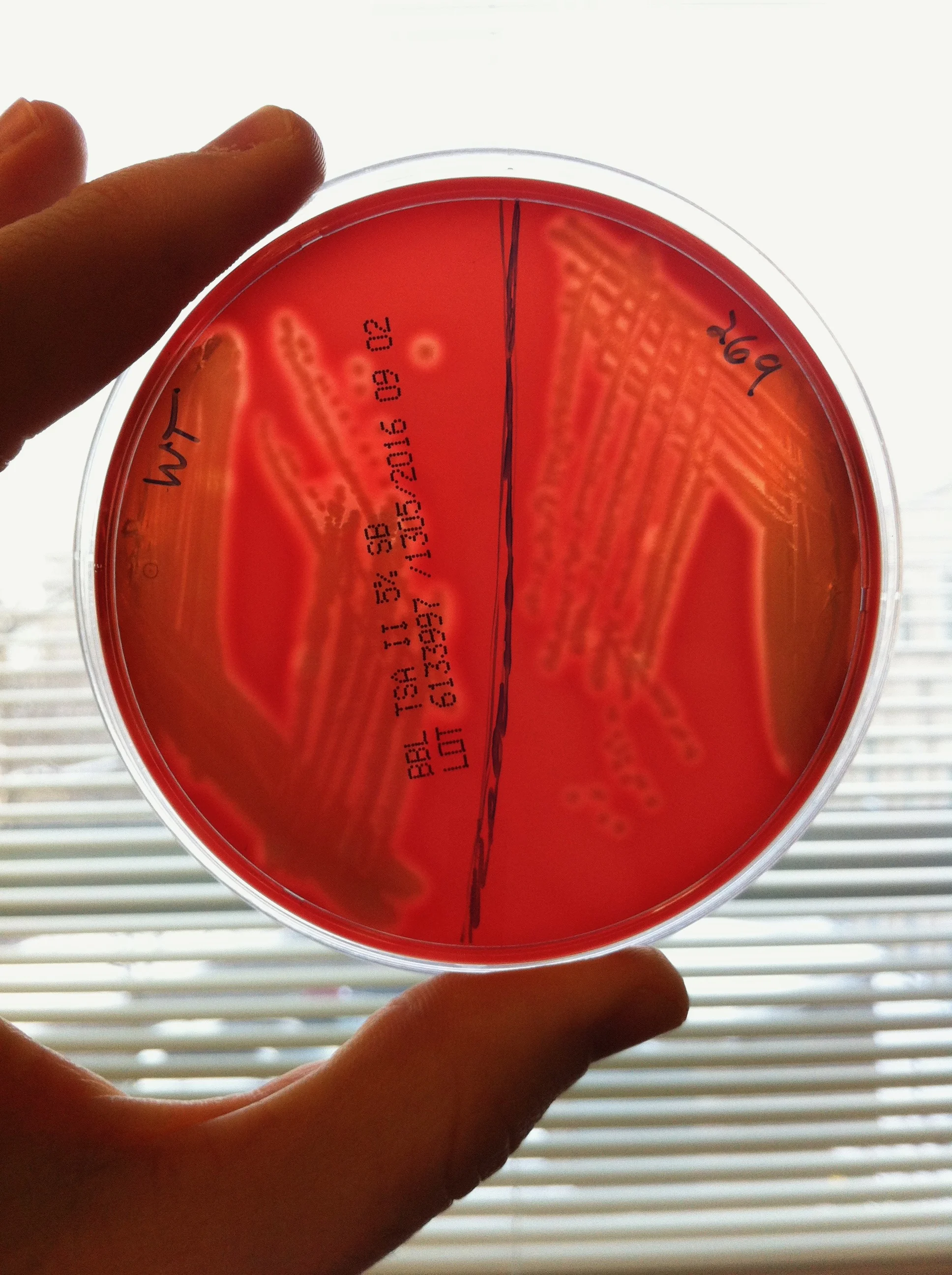
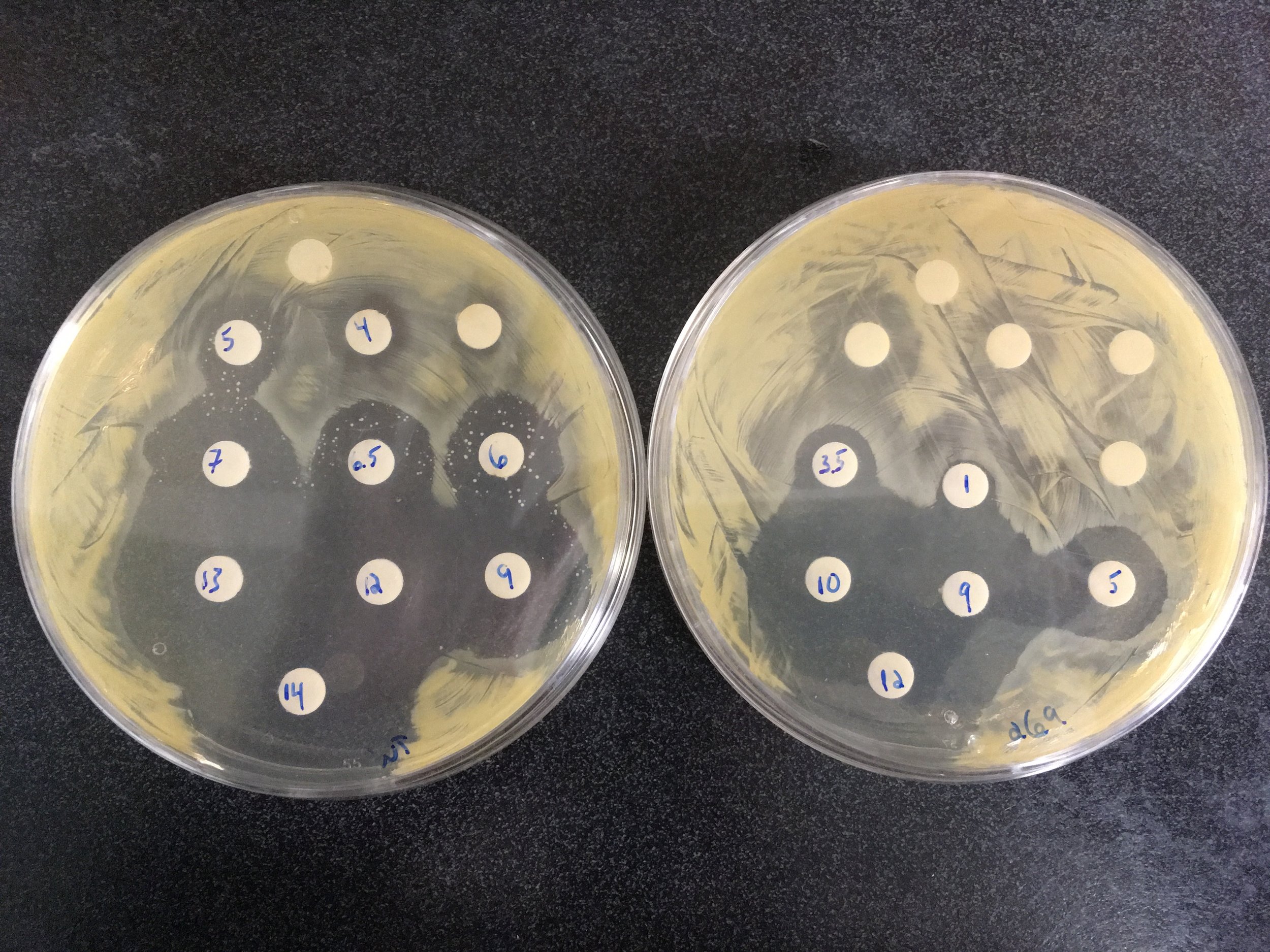
Chin D, Goncheva MI, Flannagan RS, Deecker SR, Guariglia-Oropeza V, Ensminger AW, Heinrichs DE. Coagulase-negative staphylococci release a purine analog that inhibits Staphylococcus aureus virulence. Nat Commun. 2021 Mar 25;12(1):1887. doi: 10.1038/s41467-021-22175-3. PubMed PMID: 33767207; PubMed Central PMCID: PMC7994395.
Watson DW, Iglesias SL, Vasarhelyi EM, Heinrichs DE. GraXRS-Dependent Resistance of Staphylococcus aureus to Human Osteoarthritic Synovial Fluid. mSphere. 2021 Mar 10;6(2). doi: 10.1128/mSphere.00143-21. PubMed PMID: 33692196; PubMed Central PMCID: PMC8546691.
Flannagan RS, Farrell TJ, Trothen SM, Dikeakos JD, Heinrichs DE. Rapid removal of phagosomal ferroportin in macrophages contributes to nutritional immunity. Blood Adv. 2021 Jan 26;5(2):459-474. doi: 10.1182/bloodadvances.2020002833. PubMed PMID: 33496744; PubMed Central PMCID: PMC7839378.